Table of Contents
Introduction
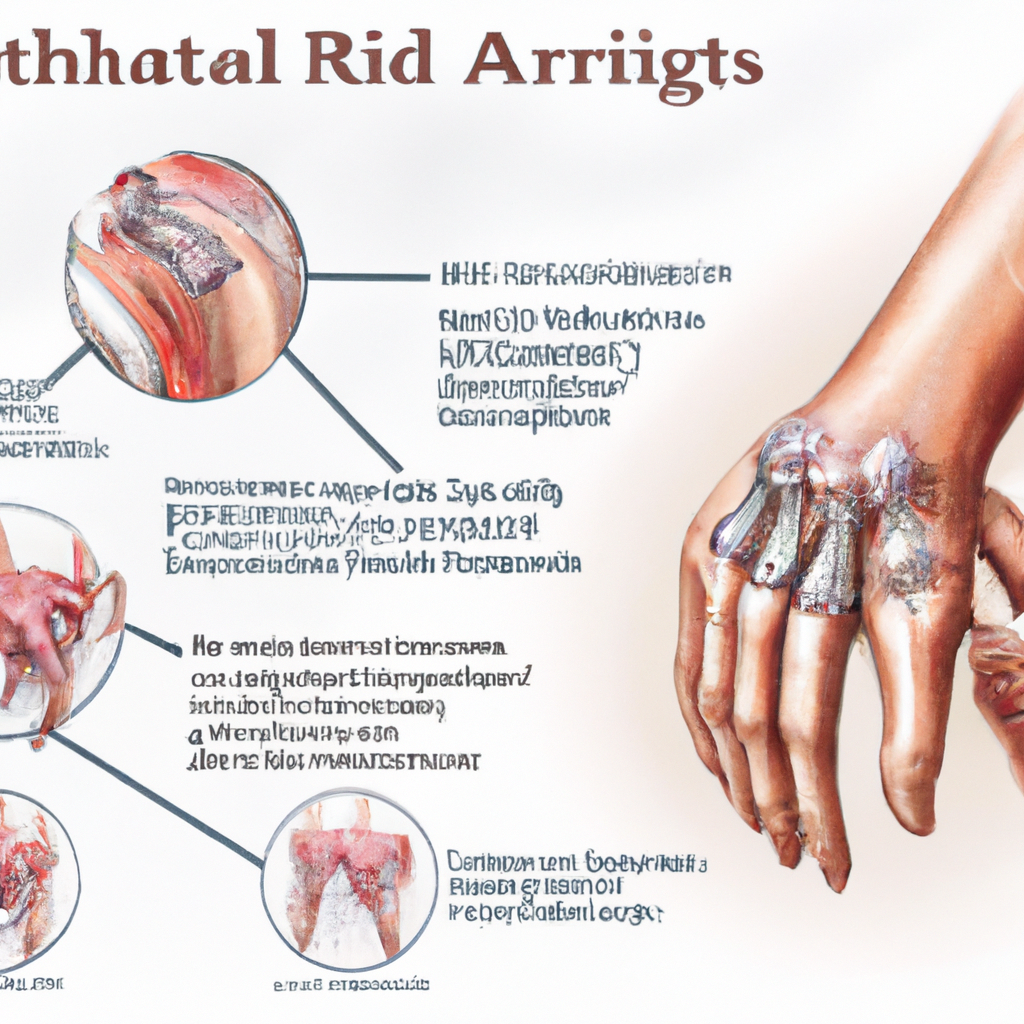
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that affects the joints and can cause severe pain, swelling, and stiffness. It is estimated that 1.3 million Americans suffer from RA, and it is the most common type of inflammatory arthritis. Understanding the causes and symptoms of RA is essential for early diagnosis and effective treatment. This article will provide an overview of the causes and symptoms of RA, as well as the potential treatments available.
Overview of Rheumatoid Arthritis: Causes and Symptoms
Rheumatoid arthritis (RA) is a chronic, inflammatory autoimmune disorder that affects the joints and other organs in the body. It is characterized by joint pain, swelling, and stiffness, and can lead to joint damage and disability if left untreated.
RA is caused by an abnormal immune response, in which the body’s own immune system attacks the joints and other organs. This results in inflammation and destruction of the joint tissue, leading to pain, swelling, and stiffness. RA can also affect other organs, such as the lungs, heart, and eyes.
The exact cause of RA is unknown, but certain factors are thought to increase the risk of developing the condition. These include genetic factors, environmental triggers, and certain lifestyle factors.
The most common symptoms of RA include joint pain, swelling, and stiffness. These symptoms usually occur in the same joints on both sides of the body, such as the wrists, elbows, and knees. Other symptoms may include fatigue, fever, weight loss, and anemia.
RA is diagnosed based on a physical examination, laboratory tests, and imaging tests. Treatment typically involves medications, physical therapy, and lifestyle changes. The goal of treatment is to reduce pain and inflammation, prevent joint damage, and improve overall quality of life.
Although there is no cure for RA, early diagnosis and treatment can help reduce the severity of symptoms and slow the progression of the disease. With proper treatment, many people with RA can lead active, productive lives.
Genetics and Environmental Factors in Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that affects the joints and other parts of the body. It is characterized by inflammation, pain, and stiffness in the joints, as well as fatigue, fever, and loss of appetite. The cause of RA is not fully understood, but both genetics and environmental factors are thought to play a role.
Genetics is believed to be a major factor in the development of RA. Studies have identified certain genes that are associated with an increased risk of developing the condition. These genes are thought to affect the body’s immune system, making it more likely to attack its own tissues. This can lead to inflammation and joint damage.
In addition to genetics, environmental factors are also thought to play a role in the development of RA. Exposure to certain toxins, such as silica dust, may increase the risk of developing the condition. Smoking has also been linked to an increased risk of RA, as well as certain infections, such as the Epstein-Barr virus.
The exact cause of RA is still unknown, but it is likely a combination of genetic and environmental factors. It is important to note that not everyone with the same genetic predisposition will develop RA, and not everyone with the same environmental exposures will develop the condition. It is also important to remember that even if someone has a genetic predisposition to RA, it does not mean that they will definitely develop the condition.
Although the exact cause of RA is still unknown, it is important to be aware of the potential genetic and environmental factors that may increase the risk of developing the condition. If you are concerned about your risk of developing RA, it is important to talk to your doctor about your family history and any potential environmental exposures. With proper diagnosis and treatment, RA can be managed and the symptoms can be controlled.
Diagnosing Rheumatoid Arthritis: Tests and Imaging
Diagnosing Rheumatoid Arthritis (RA) can be a complex process, as there is no single test that can definitively diagnose the condition. A combination of tests and imaging is used to determine if a person has RA and to what extent.
The first step in diagnosing RA is a physical exam. During the exam, the doctor will look for signs of inflammation, such as redness, warmth, and swelling. They will also check for joint tenderness and stiffness. The doctor may also check for signs of muscle weakness and any other physical signs that may indicate RA.
The next step is to perform a series of blood tests. These tests can help to identify certain markers that are associated with RA, such as rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies. These tests can also help to rule out other conditions that may have similar symptoms.
Imaging tests can also be used to diagnose RA. X-rays can help to identify joint damage that is caused by RA. Magnetic resonance imaging (MRI) and ultrasound can also be used to assess the extent of joint damage.
Finally, a doctor may refer a patient to a rheumatologist for further evaluation. A rheumatologist is a doctor who specializes in the diagnosis and treatment of RA. The rheumatologist may perform additional tests and imaging to confirm the diagnosis and to assess the severity of the condition.
The diagnosis of RA is a complex process that requires a combination of tests and imaging. The physical exam, blood tests, and imaging tests can all help to identify the presence of RA and to assess the extent of joint damage. A referral to a rheumatologist may also be necessary to confirm the diagnosis and to determine the best course of treatment.
Treating Rheumatoid Arthritis: Medications and Therapies
Treating Rheumatoid Arthritis (RA) is an ongoing process that involves a combination of medications and therapies. The goal of treatment is to reduce inflammation, relieve pain, improve function, and prevent further joint damage.
Medications are the mainstay of RA treatment. Nonsteroidal anti-inflammatory drugs (NSAIDs) are the most commonly prescribed medications for RA. They work by reducing inflammation and pain. Common NSAIDs include ibuprofen, naproxen, and celecoxib. Other medications used to treat RA include corticosteroids, disease-modifying antirheumatic drugs (DMARDs), and biologic agents. Corticosteroids are powerful anti-inflammatory drugs that can be taken orally or injected directly into the joint. DMARDs work by slowing the progression of RA and can be taken orally or intravenously. Biologic agents are genetically engineered proteins that block the action of certain proteins involved in inflammation.
In addition to medications, physical and occupational therapies can help improve joint function and reduce pain. Physical therapy involves exercises that help strengthen the muscles around the joints and improve range of motion. Occupational therapy focuses on teaching patients how to use their joints safely and effectively.
Other treatments for RA include lifestyle changes. Eating a healthy diet, getting regular exercise, and managing stress can help reduce inflammation and improve overall health. In addition, some people find that alternative therapies, such as acupuncture, yoga, and massage, can help reduce pain and improve function.
Treating RA is a complex process that requires a combination of medications, therapies, and lifestyle changes. It is important to work with your doctor to develop an individualized treatment plan that meets your needs. With the right treatment, you can manage your RA and live a full and active life.
Living with Rheumatoid Arthritis: Managing Symptoms and Quality of Life
Living with Rheumatoid Arthritis (RA) can be a difficult and painful experience. RA is an autoimmune disorder that causes inflammation in the joints, resulting in pain, stiffness, and swelling. It can also cause fatigue, difficulty sleeping, and other physical and emotional symptoms. While there is no cure for RA, there are ways to manage symptoms and improve quality of life.
The first step in managing RA is to understand the condition and its symptoms. Knowing what to expect can help you plan ahead and make lifestyle changes to reduce pain and discomfort. Working with a doctor to create a personalized treatment plan is also important. Treatment plans may include medications, physical therapy, lifestyle changes, and other treatments.
Medications are an important part of RA treatment. Non-steroidal anti-inflammatory drugs (NSAIDs) are often used to reduce inflammation and pain. Disease-modifying antirheumatic drugs (DMARDs) can help slow the progression of RA and reduce joint damage. Biologic drugs, which are made from living cells, can also be used to reduce inflammation and pain.
Physical therapy is another important part of RA treatment. Physical therapists can help you develop an exercise program that is tailored to your needs. Exercise can help reduce pain and stiffness, improve joint function, and increase strength and flexibility.
Making lifestyle changes can also help manage RA symptoms. Eating a healthy diet, getting enough rest, and managing stress can all help reduce inflammation and pain. Quitting smoking, if you are a smoker, can also help reduce inflammation and improve joint health.
Living with RA can be challenging, but there are ways to manage symptoms and improve quality of life. Working with a doctor to create a personalized treatment plan, taking medications as prescribed, and making lifestyle changes can all help reduce pain and improve overall health. With the right treatment plan, it is possible to live a full and active life with RA.
Conclusion
Rheumatoid arthritis is a serious autoimmune disorder that can cause severe pain and disability. Understanding the causes and symptoms of this condition is essential for proper diagnosis and treatment. While the exact cause of RA is unknown, it is believed to be triggered by a combination of genetic and environmental factors. Common symptoms include joint pain, stiffness, swelling, and fatigue. Early diagnosis and treatment can help reduce the severity of symptoms and improve quality of life. With the right care and support, those living with RA can lead full and active lives.